OA Ing. Dr. med. univ. Thomas Johann Vögele MSc 1 | Axel Peter Prodinger MD 2
Citation / Download article as a PDF:
Vögele, T. J., & Prodinger, A. P. (2019). Osteopathic Treatment of Patients with Coxarthrosis: A Randomised Controlled Trial. European Journal of Osteopathic Research, 1(1), 8–16. https://doi.org/10.35740/EJOR.2019.1.1.2 Cite Download
Abstract
Background: The study aimed to deliver valid data for the short-term effect of osteopathic manual treatments for patients with advanced osteoarthritis of the hip.
Methods: For this prospective, randomised controlled trial patients diagnosed with coxarthrosis were randomly allocated to an intervention group and a control group. The patients in the intervention group received osteopathic treatment on three occasions for nine weeks. The control group did not receive any treatment. At the beginning and the end of the study, all patients had to specify their level of pain in general, whether they felt pain at walking, when climbing stairs and when lying. In addition, patients were questioned about restrictions in their daily activities.
Results: For the level of pain in general, the arithmetic mean of the intervention group (n = 15) decreased from 5.333 points (SD 1.589) at the start of the treatment (on a scale from 1 to 10) to 4.733 points (SD 1.534) at the end of the study. This represents a statistically significant change (p = 0.047). The other parameters improved for the patients who received osteopathic treatment, although they did not reach the level of significance. The control group (n = 15) had the same measurements from the beginning to the end of the study.
Conclusions: Only a small segment of the outcome reached statistical significance. Nevertheless, a beneficial impact of the osteopathic treatment for patients with coxarthrosis was observed. Further research should carefully consider the methods and design needed to reach statistically significant outcomes.
Keywords: arthritis, coxarthrosis, hip, OMT, osteoarthritis, osteopathy
DOI: https://doi.org/10.35740/EJOR.2019.1.1.2
Background
Osteoarthritis of the hip (coxarthrosis) is a chronic degeneration of the cartilage of the joints. The disease increases in prevalence with age. In Austria, more than a million people suffer from arthritis [1]. Pain is the main complaint for patients with coxarthrosis. In addition, these patients sometimes have difficulties coping with the demands of their everyday life. The high prevalence is even considered as a factor in national economics [2].
The damage to the joints cannot be cured, but the effects of pain and restriction of motion can be treated. At best, the progress of the disease can be delayed by therapeutic intervention. Eventually, a surgical procedure could provide relief for patients but with all the attendant risks of surgery involved.
Several studies have examined the effects of different treatment methods. Hence, it appears certain that movement therapy, Masai barefoot technology and acupuncture can ease the pain of patients with coxarthrosis [3–6]. Likewise, therapeutic exercise programmes can reduce pain and improve physical function among patients with symptomatic hip osteoarthritis [7].
The present study aimed to deliver valid data for the positive effect of osteopathic manual therapy for patients with coxarthrosis. The outcome supplements existing research papers in this field [8,9].
Methods
This prospective, randomised, controlled trial was carried out to explore the effects of osteopathic therapy with regard to pain level in general, at walking, climbing stairs, and when lying. In addition, we examined the effects of therapy about patient limitations when doing domestic activities, getting out of bed, getting on and off the toilet and doing the shopping.
The study aimed to test the null hypothesis that for patients with osteoarthritis of the hip, osteopathy has no influence on the pain felt and their ability to function in daily life.
For this purpose, 36 patients were enrolled by an orthopaedic surgeon. The participants were required to have been diagnosed with osteoarthritis of the hip grade 2 or 3 using the Kellgren and Lawrence score [10]. Additional inclusion criteria were a minimum age of 50 years and a minimum of 4 points for indicated pain. The method of grading pain used in this study was a numerical value from 1 to 10 for the severity of the pain. The restrictions were graded in 5 steps from “none” to “extreme”. The WOMAC-osteoarthritis index and the HOOS-Score served as a template [11,12]. Both internationally recognised and validated questionnaires were adapted, simplified and reduced to 4 questions each. Also, basic data were collected such as age, sex and body mass index.
Fifty-two patients who met the inclusion criteria had a personal briefing. Finally, 36 patients signed the consent form, received a patient number and were equally allocated to an intervention group and a control group by using an online randomisation tool.
The questionnaires with basic data were completed by the participants at the beginning of the study, while the questionnaires regarding the parameters were completed at the beginning and end of the study.
The participants in the intervention group received osteopathic treatment by the author of the study. Each patient in this group received three individual manual osteopathic treatments (OMT) at intervals of 3 weeks. The interventions were conducted at the author´s private practice in Styria from May to December 2016. The patients in the control group did not receive any treatment (waiting group). Neither group was allowed to take pain-killers or any other kind of medical treatment during the whole study period. The participants of the control group were offered the same osteopathic procedures after completing their questionnaires following the nine weeks waiting period, that is, after the end of the study.
At the start and end of the study, all participants had to specify their sensation of pain (general feeling of pain, pain at walking, climbing stairs and when lying down) and their restrictions in function (when doing domestic duties, getting out of bed, getting on and off the toilet and doing the shopping).
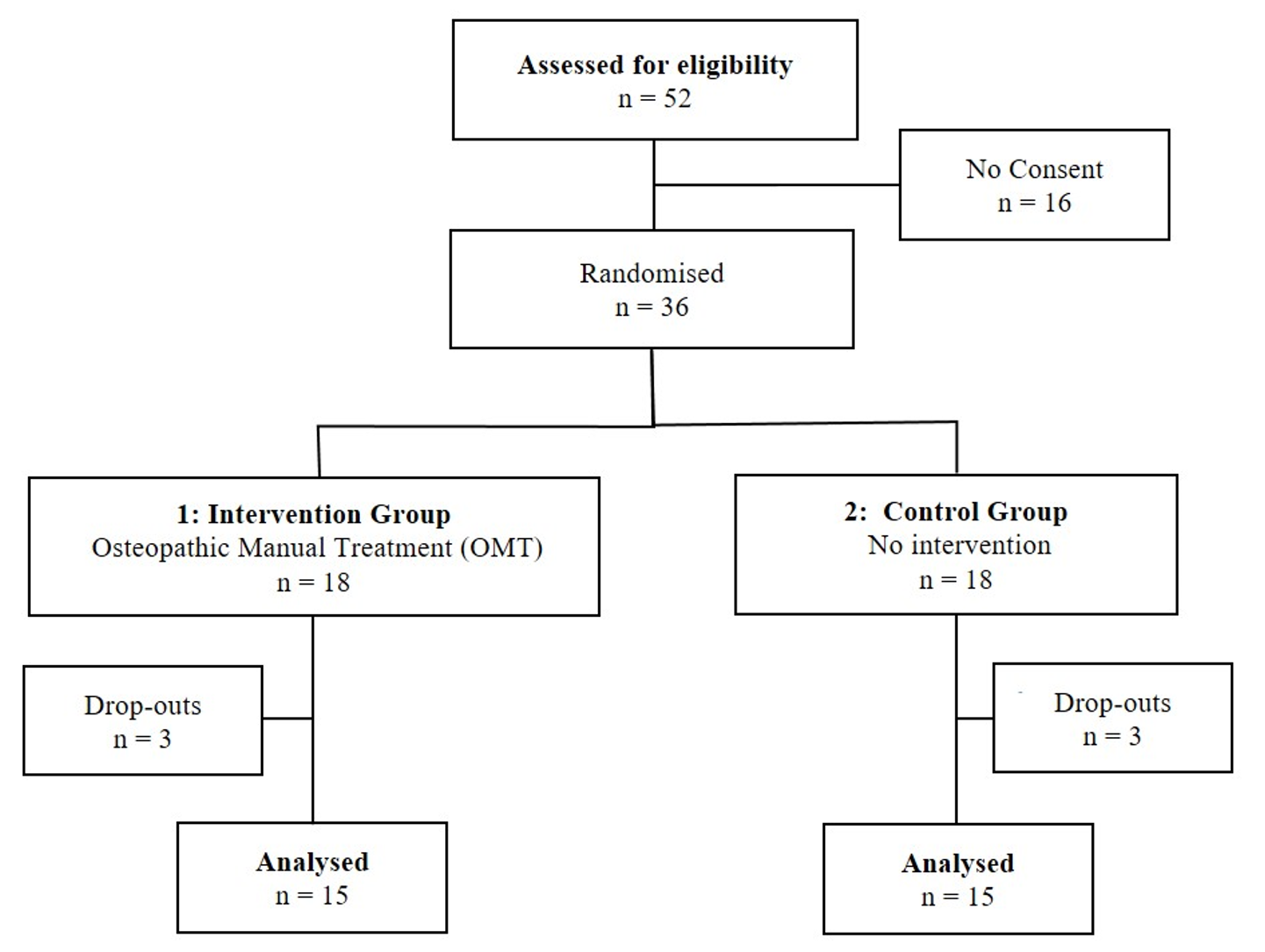
Figure 1: Participant flow
Baseline characteristics of the patients entering the study were balanced between the two groups.
Of the 18 patients, three patients in the intervention group dropped out: one patient started a stay at a health resort, one patient had surgery, and another was sceptical about osteopathy. The control group was also reduced to 15 participants: 2 patients took pain killers during the study period, and one patient could not be reached for further appointments. Therefore, the data of 15 participants per group could be analysed.
Statistics
Subsequent to the descriptive statistics, the arithmetic mean was calculated for metric scaled characteristics. The normal distribution was tested. To compare the groups, the t-test was used.
Analysis of variance was performed to test the differences of the means followed by post-hoc tests. The Wilcoxon signed-rank test was used for non-normal, dependent samples, and the Mann-Whitney U-test for independent samples. Differences in frequency were tested using Pearson’s chi-square test.
Correlation analyses were used to find potential correlations. The significance level was set at 5%; that is, a p-value smaller than 0.05 was considered significant.
Results
The study examined the changes of the primary and secondary parameters resulting from 3 osteopathic treatments for patients with coxarthrosis.
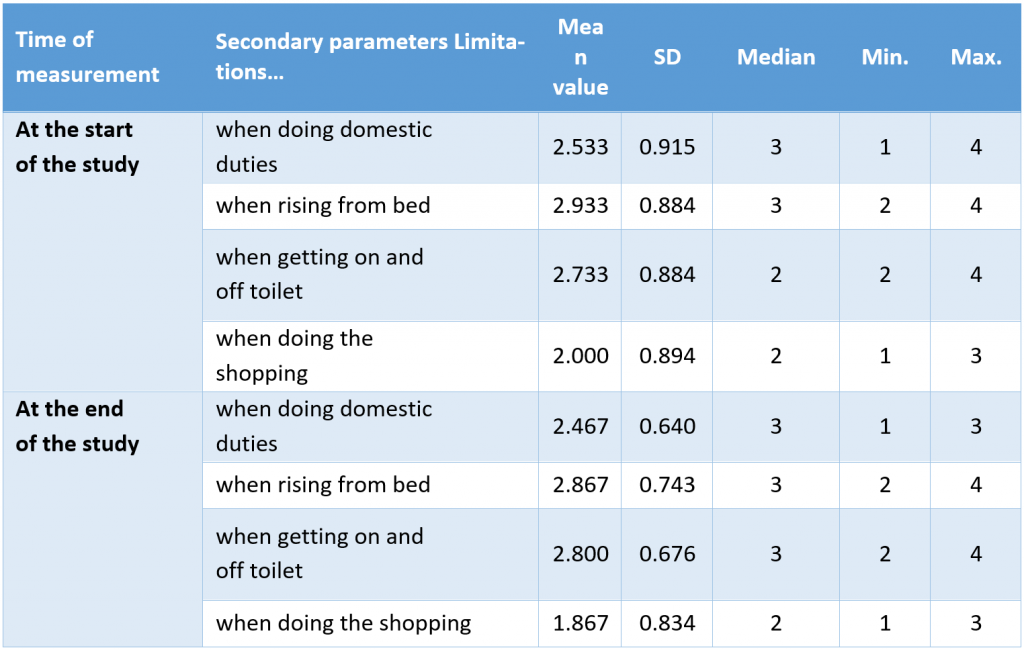
Figure 1 shows the number of participants during the study phases. Tables 1 – 4 show the values for primary and secondary parameters at the start and end of the study.
Table 1: Statistical key values for the intervention group for primary parameters
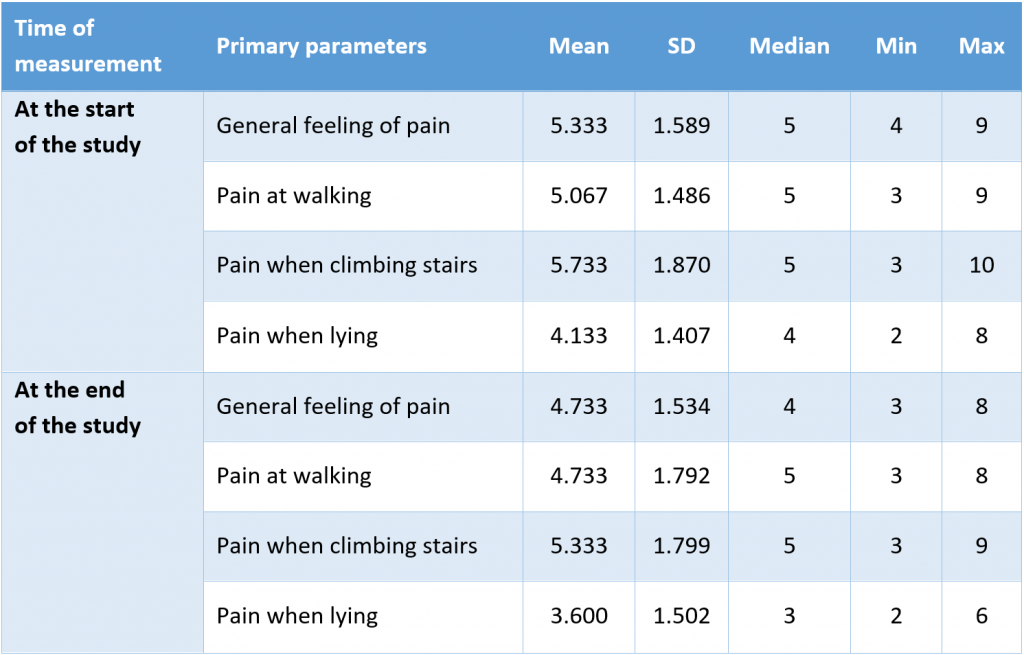
Table 2: Statistical key values for the control group for primary parameters
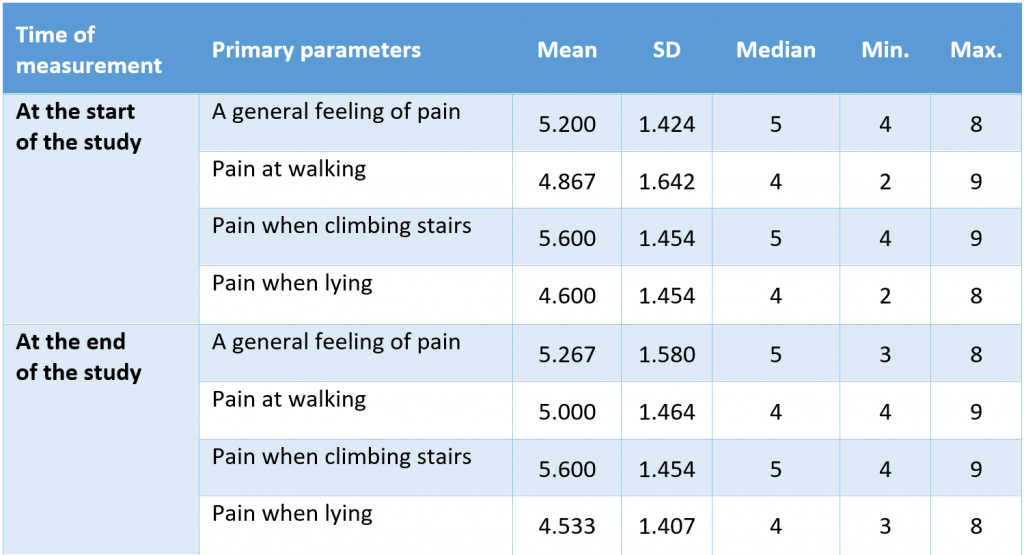
Table 3: Statistical key figures for the intervention group for secondary parameters
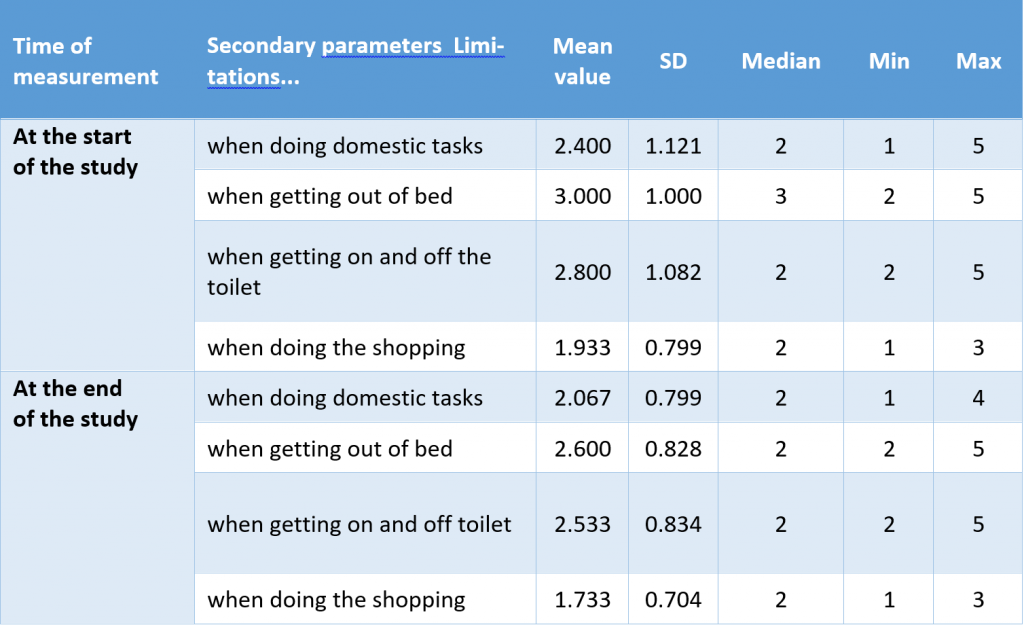
Table 4: Statistical key figures for the control group for secondary parameters
Taking the general feeling of pain as an example, the figures show that the arithmetic mean of the intervention group is 5.333 points (SD 1.589) at the start of the study and is similar to the average mean of the intervention group with 5.200 points (SD 1.424). At the end of the study, the mean value decreases for the intervention group to 4.733 points (SD 1.534) and is nearly stable with 5.267 points (SD 1.580) for the control group (see also Figure 2). All other parameters show a comparable pattern.
Table 5: Comparison of the values at the start and the end of the study for all parameters. *: significant difference (p < 0.05)
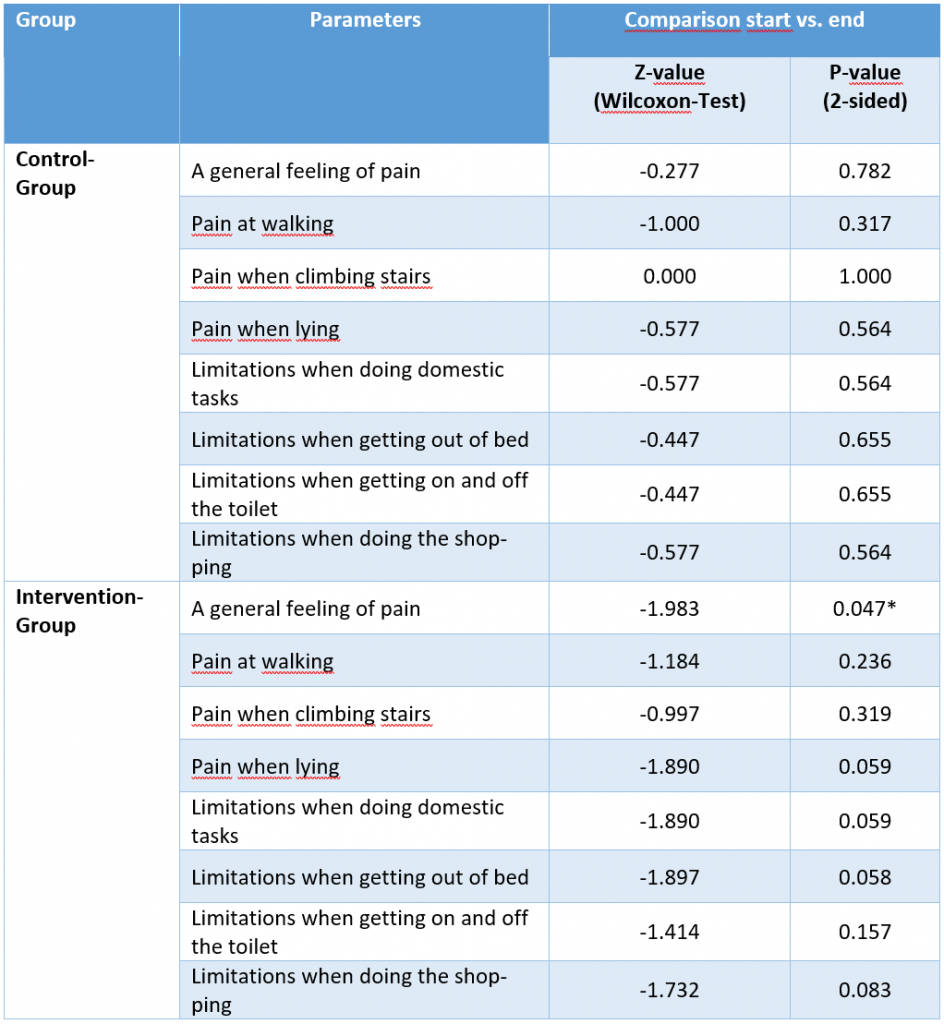
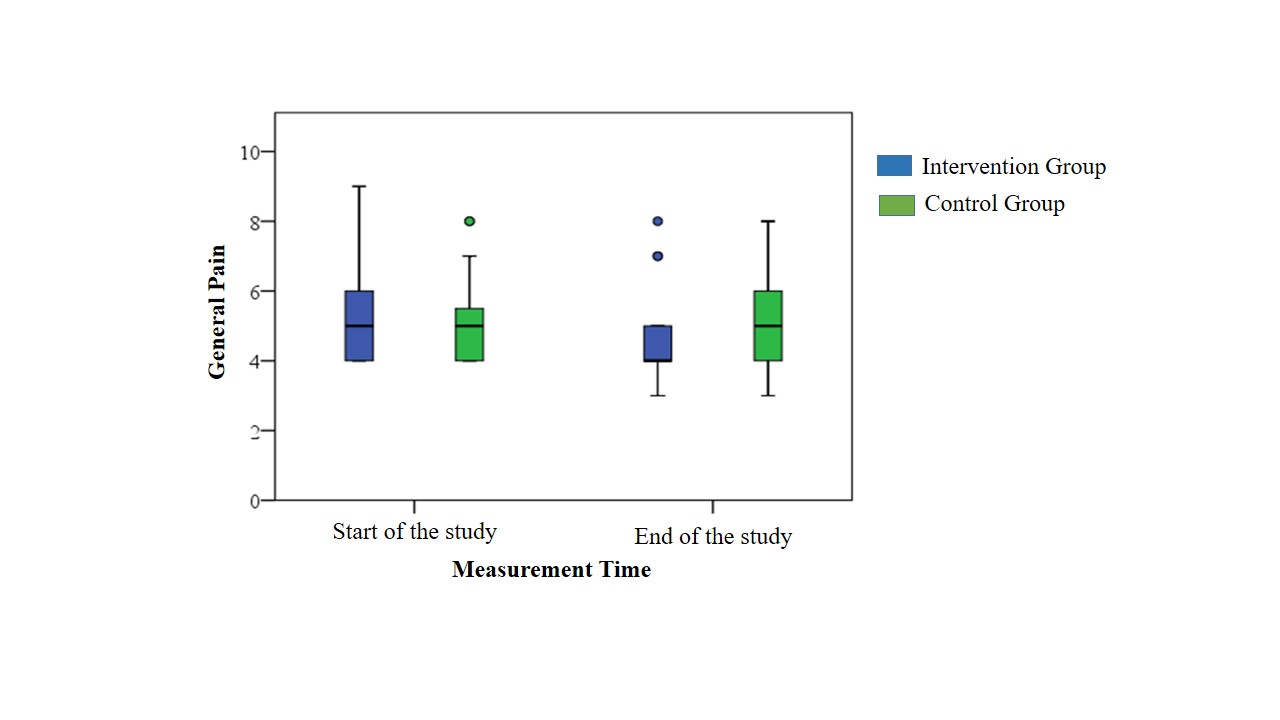
Figure 2: Boxplot: General level of pain for each group
Comparing the values at the start of the study with the values at the end of the study for each group shows a similar picture (see Table 5). Only one parameter reaches the level of significance. The value for the general level of pain decreases in the intervention group from a median of 5 to a median of 4 at the end of the study (p = 0.047). All other changes remain below the level of significance (< 0.05).
Discussion
Interpretation of the results
The study aimed to answer the question whether three osteopathic treatments during nine weeks improve the general feeling of pain and the restrictions in daily activities for patients with coxarthrosis. The results indicate that from a statistical point of view, the research question is to be answered in the negative. The null hypothesis that osteopathy has no influence on patients with osteoarthritis of the hip with regard to the general feeling of pain and ability to function in daily activities cannot be rejected. Only a single parameter out of 8 showed a statistical significance. Therefore, we cannot positively confirm the research question.
Nevertheless, the outcomes clearly show the tendency for osteopathic treatment to positively influence the quality of life for patients with coxarthrosis.
Somatic dysfunction and coxarthrosis
The participants of this trial suffered from a diagnosed coxarthrosis grade 2 or 3 and had an average age of 70 years. Osteoarthritis is a degenerative disease leading to progressive and irreparable damage of the hip joint [13–15]. Primary osteoarthritis is associated with ageing and has no known specific cause [16]. From an osteopathic point of view, a somatic dysfunction most probably influences and stimulates the destruction process of the cartilage. Therefore, especially for primary coxarthrosis, where no obvious cause for the disease can be identified, the most effective therapy would have been the preventive treatment of the so-called impaired or altered function of related components of the somatic (body framework) system which led to the damage [17]. Once the joint is in poor condition, osteopathic treatment is more or less restricted to damage control. Hence, reliable statements about the positive effect of osteopathy are reported mainly for disorders that are not based on irreversible damage [18].
In a nutshell, coxarthrosis in an advanced stage does not represent an ideal basis to demonstrate the potential of osteopathic treatment.
Intersubjectivity
The author chose to treat each patient individually without a given defined and standardised procedure. This meets the requirements of osteopathic manual treatment (OMT), which is the therapeutic application of manually guided forces by an osteopath to improve physiological function and/or support homeostasis that has been altered by somatic dysfunction. Practitioners of OMT employ a variety of techniques [17]. The osteopath has to decide on a case-by-case basis on the suitable structural, visceral or cranial techniques to apply. Therefore, a particular osteopath might apply different techniques with possibly slightly different effects. This freedom of choice does compromise the quality criteria of intersubjectivity, and it cannot be guaranteed that another osteopath would obtain the same results.
Preceding studies
A comparable study examined the effect of 6 osteopathic treatments [8). The outcome was altogether positive. However, upon closer examination, the participants do not have enough parallels to allow a serious comparison with our study. The age of the participants ranged from 20 to 50 years. The composition of the study population is questionable because primary coxarthrosis generally occurs at the age of 50 years or later [14]. The average age of the patients in our study is 70 years. With regard to these considerations, no further comparisons could be made.
A second study in this field examined whether the various forms of the complaints of coxarthrosis can be influenced by an osteopathic treatment [9]. After a waiting period of 6 weeks, 30 patients with diagnosed coxarthrosis in stage 1 or 2 were treated on four occasions. The results showed a very significant improvement of the values for pain, restrictions in daily life and quality of life. However, even without any treatment, an improvement was recorded immediately after the waiting period. In addition, the average age was 55 years and therefore, nearly 15 years below the average of this study. Moreover, the patients were enrolled at an earlier stage of the illness. As mentioned before, it seems to be easier to demonstrate a statistically significant effect for osteopathic treatment for an earlier stage of damage.
Conclusions
Summary
This study aimed to demonstrate that osteopathy could reduce pain and improve physical function among patients with coxarthrosis. This assumption could not be verified statistically. However, from a subjective point of view, the patients in the intervention group had less pain and better physical function by the end of the study.
Outlook
Considering the increasing prevalence of coxarthrosis and the impaired quality of life of patients with this disease, further studies should be conducted given the potential of osteopathic treatment.
Future examinations should emphasise preventive measures to gain the greatest effect. Solving somatic dysfunctions could have an impact on the time and intensity of disease occurrence. Accordingly, long-term studies would be very interesting.
Another aspect that seems to be of importance is the holistic approach of osteopathy. Osteopathic treatment can only trigger the healing process. The patient’s attitude is crucial for the success of the therapy. The author is convinced that the positive effects would increase if participants enrolled were those who accepted responsibility for their healthcare and have a positive attitude. This factor should be considered for the selection criteria for future studies.
Discloser
The authors have no personal financial or institutional interest in any of the drugs, materials or devices described in this article.
Author details
1 Rudolfinerhaus Privatklinik GmbH, Austria
2 LKH Stolzalpe, Austria
Correspondence
Dr Thomas Vögele, Urbangasse 6/3/40, 1170 Wien, Austria
Email: dr.voegele@osteomed.at
Received: 20 August 2019 Accepted: 21 November 2019 Published: 26 November 2019
References
1. Baldaszti E, Statistik-Austria, editors. Jahrbuch der Gesundheitsstatistik – Bundesanstalt Statistik Austria. Wien: Verlag Österreich GmbH; 2015.
2. Engelhardt M. Epidemiologie der Arthrose. Dtsch Z Für Sportmed. 2003;54[6):171–5. Researchgate
3. Abbott JH, Robertson MC, Chapple C, Pinto D, Wright AA, Leon de la Barra S, et al. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee. Osteoarthritis Cartilage. 2013 Apr;21[4):525–34. https://doi.org/10.1016/j.joca.2012.12.014
4. Krauß, I., Steinhilber, B., Haupt, G., Mille, R., Martus,P., Janßen, P. Sporttherapie bei Coxarthrose – Eine randomisierte kontrollierte Studie. Int 2014. 2014;[111):592–9. DOI: 10.3238/arztebl.2014.0592
5. Bendig AC. Wirkung einer zehnwöchigen Trainingsintervention mit der Masai Barfuß Technologie [MBT) auf Schmerzverhalten, Lebensqualität, Gleichgewichtsfähigkeit, Kraftausdauer und Beweglichkeit bei Patienten mit Hüftarthrose oder implantiertem Hüftgelenk [Internet] [Dissertation]. Universität Tübingen; 2006 [cited 2016 Jul 6]. Available from: https://publikationen.uni-tuebingen.de/xmlui/handle/10900/44890
6. Fink M, Karst M, Wippermann B, Gehrke A. Akupunktur als komplementäres Behandlungsverfahren in der Physikalischen Medizin am Beispiel der Koxar-throse. Phys Med Rehabil Kurortmed. 2001 Aug;11[04):123–8. https://doi.org/10.1055/s-2001-16442
7. Fransen M, McConnell S. Landbased Exercise for Osteoarthritis of the Knee: A Metaanalysis of Randomized Controlled Trials. J Rheumatol. 2009;36[6):1109–17. https://doi.org/10.3899/jrheum.090058
8. Bergthaler H. Objectively and subjectively observed changes in patients diag-nosed with primary coxarthrosis following osteopathic treatment with and without supplemental glucosaminesulfate and MSM. [Wien, Österreich]: Wiener Schule für Osteopathie – WSO; 2003.
9. Kießling G, Trantenroth M. Die osteopathische Behandlung der Coxarthrose. [Deutschland]: Akademie für Osteopathie; 2004.
10. Kellgren JH, Lawrence JS. Radiological Assessment of Osteo-Arthrosis. Ann Rheum Dis. 1957 Dec;16[4):494–502.
11. Stucki G, Meier D, Stucki S, Michel BA, Tyndall AG, Dick W, et al. Evaluation of a German version of WOMAC [Western Ontario and McMaster Universities) Arthrosis Index. Z Rheumatol. 1995;55[1):40–9. DOI: 10.1136/ard.16.4.494
12. Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteo-arthritis outcome score [HOOS) – validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:1–8. DOI: 10.1186/1471-2474-4-10
13. Ficklscherer A. BASICS Orthopädie und Traumatologie. 4th ed. München: Ur-ban & Fischer Verlag/Elsevier GmbH; 2014. 144 p.
14. Breusch S, Clarius M, Mau H, Sabo D. Klinikleitfaden Orthopädie Unfallchi-rurgie. 7th ed. München: Urban & Fischer Verlag/Elsevier GmbH; 2013. 960 p. https://doi.org/10.1016/b978-3-437-22473-7.05001-9
15. Debrunner AM. Orthopädie /Orthopädische Chirurgie. Patientenorientierte Diagnostik und Therapie des Bewegungsapparates. 4., vollst. neu bearb. Aufl. 2005. Bern: Huber, Bern; 2005. 1261 p.
16. Klein C. Orthopädie für Patienten: Medizin verstehen. Wirbelsäule, Halswirbelsäule, Brustwirbelsäule, Brustkorb, Lendenwirbelsäule, Schulter, Ellenbogen, Hand, Hüfte, Knie, Fuss. 1st ed. Remagen: Verlag Michels-Klein; 2014. 827 p.
17. Glossary of Osteopathic Terminology [Internet]. Educational Council on Osteopathic Principles [ECOP), American Association of Colleges of Osteopathic Medicine [AACOM). 2011 [cited 2016 Jun 26]. Available from: http://www.aacom.org/docs/default-source/insideome/got2011ed.pdf?sfvrsn=2
18. Haas NP, Hoppe J-D, Scriba PC. Wissenschaftliche Bewertung osteopathischer Verfahren. Dtsch Ärzteverlag GmbH. 2009;106[46):2325–634.
